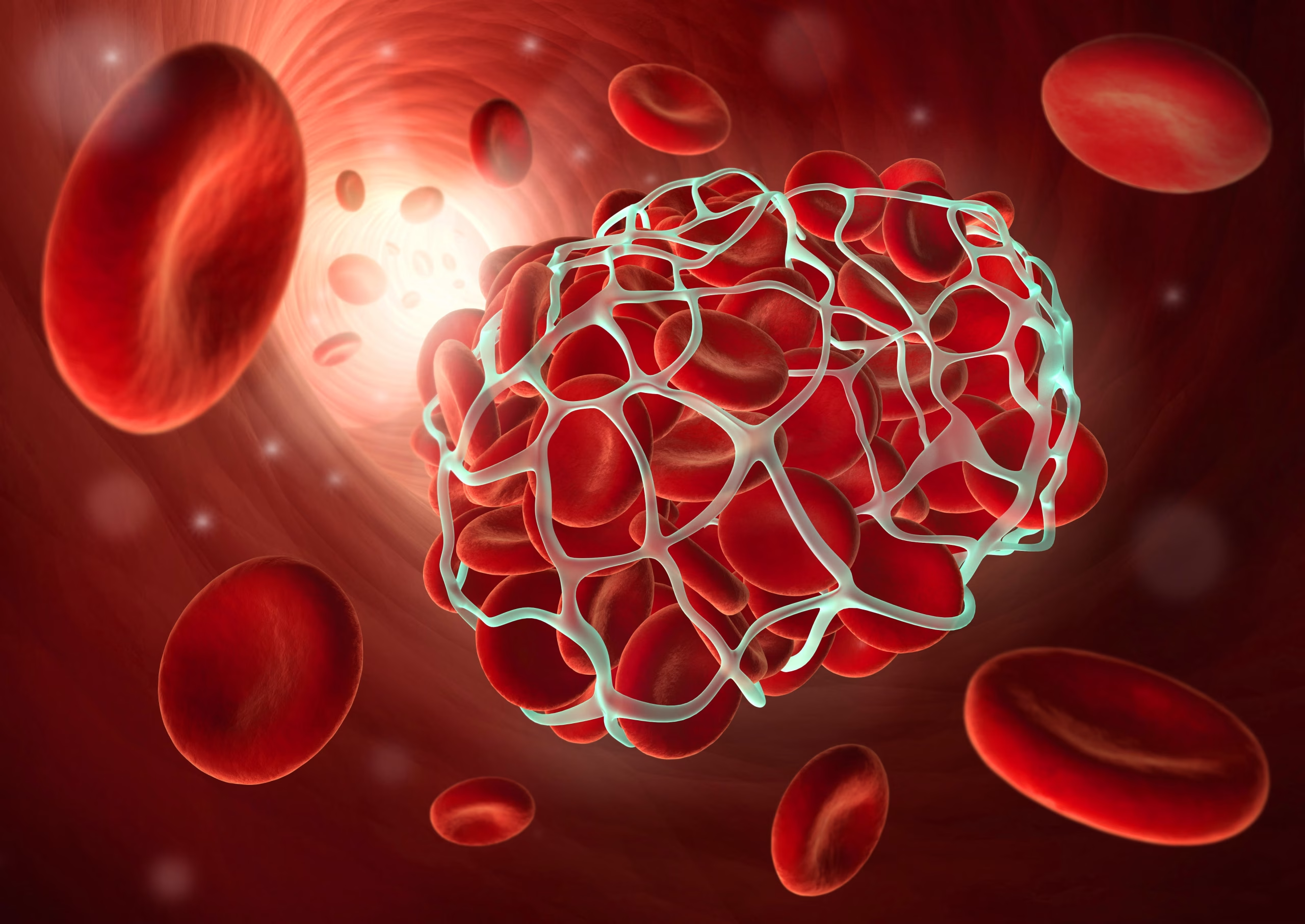
You think it’s just soreness. Maybe from sitting too long. A tight calf. A dull ache. You stretch. It doesn’t help. Then it feels warmer. Firmer. Still, no injury. The skin starts to swell. Pressure builds. That’s when the clot becomes visible—not outside, but in sensation.
Deep vein thrombosis hides behind symptoms most people dismiss during busy weeks
You walk less. Travel more. A plane ride. A long meeting. A minor sprain. These build the setting. DVT doesn’t require trauma. It forms silently. Blood pools in the legs. Movement slows. The vein narrows. The clot anchors—and sometimes, it stays unnoticed for days.
Pain that doesn’t change with movement begins to feel more suspicious with each passing hour
A pulled muscle improves when you rest. A clot doesn’t. Elevation helps briefly. But the pressure returns. Walking hurts more, not less. You ice it. Nothing shifts. The discomfort deepens instead of fading. That reversal often signals something internal—not structural.
Redness and swelling that spreads rather than stays still raises more concern than bruising ever does
Bruises fade. Clot-related redness spreads. Especially around the calf or inner thigh. The leg looks different. Side by side, the change shows. One larger. One warmer. The skin tightens. Socks leave deeper lines. Compression increases awareness—not relief.
A clot in the lung doesn’t announce itself—it begins with shortness of breath that doesn’t match exertion
You climb stairs. Suddenly you gasp. You walk down the hall. Your chest tightens. This isn’t asthma. Or anxiety. The breathing shifts without warning. You stop. Sit. Wait. The discomfort stays. That’s often a pulmonary embolism forming its first signal.
Coughing without illness, especially with blood-streaked sputum, points toward something urgent
You’re not sick. No cold. No fever. Yet you cough. It burns. You check the tissue. Red appears. It’s slight—but it matters. That’s blood from the lungs. A small clot may have traveled. You won’t always collapse. But your lungs are warning softly.
Rapid heartbeat in the absence of fever or stress often follows unnoticed clot movement
You feel your pulse. It’s racing. No heat. No panic. No exercise. Just speed. The body compensates. The heart pushes harder. It senses blockage somewhere. Your breath shortens. The pulse keeps climbing. This isn’t nerves. It’s the system reacting.
Clots can form post-surgery, even with compression stockings and mobility routines in place
You follow every rule. You walk early. Wear the socks. Do the breathing exercises. But still, days later—swelling. Clots form despite caution. Especially with orthopedic surgery. Pelvic procedures. Abdominal trauma. Healing brings risk. Not just relief.
Birth control, pregnancy, and hormone therapy increase clotting risk more than most expect
Estrogen changes clotting factors. The blood thickens slightly. Alone, it’s manageable. But add travel, immobility, smoking, or genetics—and risk rises. Hormonal balance shifts the body. The veins respond differently. Young age doesn’t always protect.
Genetic clotting disorders often remain silent until stress or surgery reveals them
You never knew. No symptoms. Then a clot after minor surgery. Or long travel. Then testing begins. Factor V Leiden. Prothrombin mutations. Protein C or S deficiencies. These remain hidden. Until the wrong condition reveals them. Then lifelong vigilance follows.
Cancer itself increases clotting risk—sometimes before it’s even diagnosed
Clots appear without cause. Then again. The pattern confuses. Further scans begin. Sometimes a tumor appears—pancreas, ovary, colon. Malignancy shifts blood chemistry. Cancer is a pro-thrombotic state. Sometimes, the clot leads to the diagnosis—not the other way around.
Compression ultrasounds confirm DVT, but not all clots can be seen without advanced imaging
You visit urgent care. They scan the leg. They may miss it. Not all clots show clearly. Small ones hide. Pelvic clots need CT or MRI. Sometimes a clean scan doesn’t mean no clot—it means it’s elsewhere. Symptoms still guide next steps.
Anticoagulants remain the first-line treatment, but dosage and duration vary based on the cause
You start blood thinners. Apixaban. Rivaroxaban. Heparin. Warfarin. Each has rules. Some need labs. Others don’t. Clot size. Location. Risk factors. All decide how long you continue. Three months. Six months. Life-long. It isn’t one plan for all.
Not every clot needs hospitalization, but all need follow-up to avoid silent recurrence
You’re stable. You’re discharged. But the clot still exists. Follow-up matters. Bloodwork. Imaging. Lifestyle shifts. Recurrence happens quietly. One clot raises your future risk. One event changes your baseline. Monitoring doesn’t end with the prescription.
Clot prevention begins with movement, hydration, and awareness—not just after diagnosis, but always
You stretch on flights. Flex calves. Walk every hour. Drink water. Watch leg swelling. These aren’t just comfort measures—they’re prevention. Clots don’t need drama to form. Stillness is their stage. You reduce risk by never staying still too long.
Source: Hematology in Dubai / Hematology in Abu Dhabi