The insidious nature of blood cancer, which encompasses malignancies like leukemia, lymphoma, and multiple myeloma, often lies in its initial clinical presentation—a subtle, unspecific constellation of symptoms easily mistaken for a routine viral infection, overwork, or the common flu. Unlike tumors that form a distinct mass and prompt an obvious localized complaint, blood cancers involve the dysfunctional proliferation of blood cells within the bone marrow, lymphatic system, or bloodstream, leading to consequences that are systemic and highly variable. Consequently, the earliest indicators are frequently vague, requiring an observant eye and a physician prepared to pursue an explanation beyond the immediately obvious, differentiating between transient illness and persistent hematological abnormality. The pathway to diagnosis is rarely straightforward, starting instead with a persistent sense of unease.
The earliest indicators are frequently vague, requiring an observant eye and a physician prepared to pursue an explanation beyond the immediately obvious, differentiating between transient illness and persistent hematological abnormality.
One of the most universally reported, yet poorly characterized, initial complaints is a profound, relentless sense of fatigue. This is not the weariness that follows a sleepless night or a stressful week, but a deep-seated, persistent exhaustion that no amount of rest or sleep seems capable of alleviating. The underlying mechanism is typically anemia, caused by the bone marrow’s inability to produce sufficient healthy red blood cells due to the overcrowding by malignant cells. These red blood cells are essential for oxygen transport, so their deficiency starves the body’s tissues of the necessary fuel, manifesting as crippling tiredness, unusual weakness, and often, noticeable paleness of the skin, a sign technically known as pallor. It is the disproportionate nature of this exhaustion relative to the patient’s activity level that should raise the first clinical suspicion, a fatigue that disrupts the flow of everyday activities in a significant, persistent manner.
This is not the weariness that follows a sleepless night or a stressful week, but a deep-seated, persistent exhaustion that no amount of rest or sleep seems capable of alleviating.
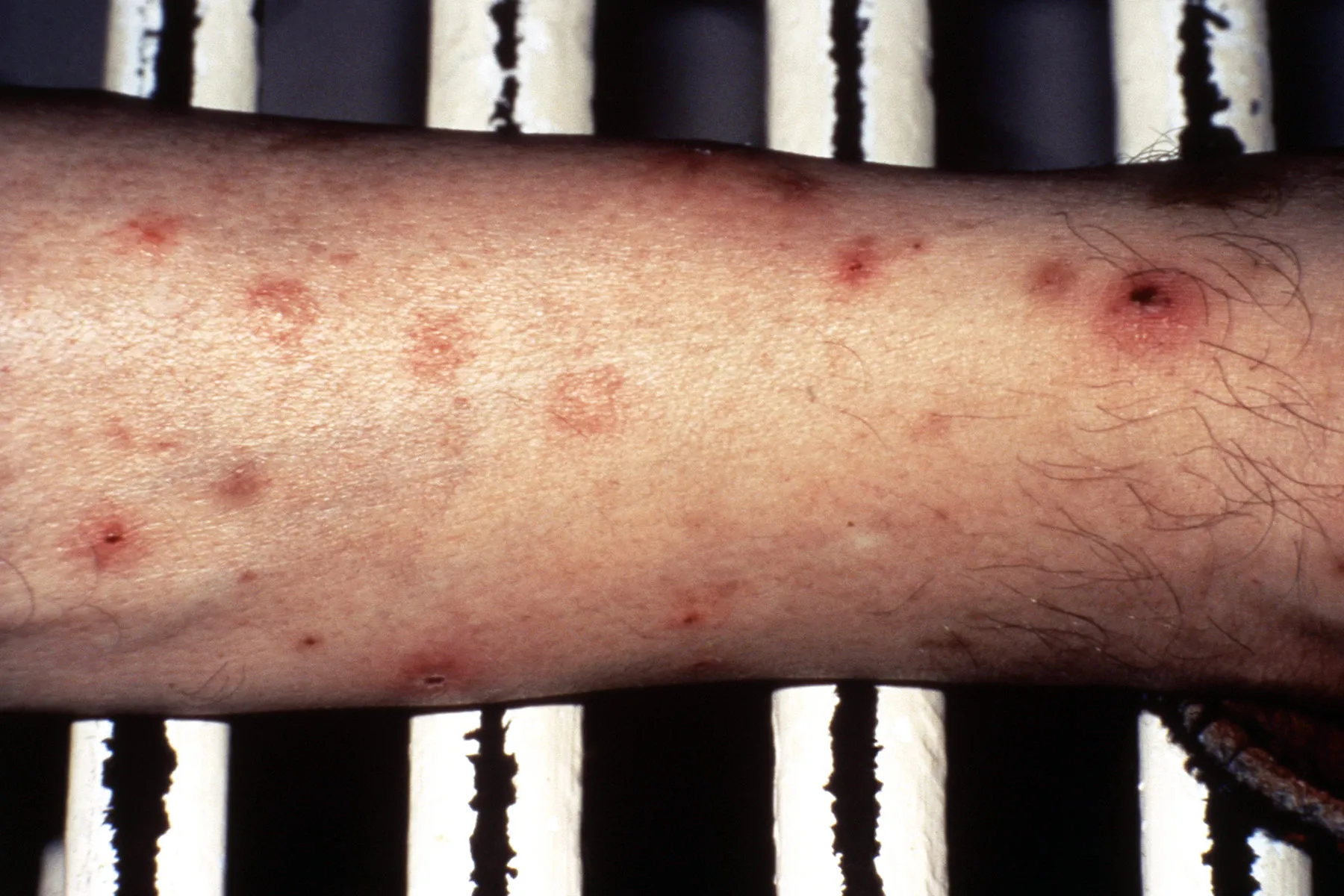
The disruption to the body’s normal blood cell production extends critically to platelets, which are the components responsible for clotting. A reduced platelet count, or thrombocytopenia, directly results in an increased propensity for bleeding and bruising, which can serve as another early and visible warning sign. Patients may start to notice bruising in unusual locations, such as the back, abdomen, or upper arms, without any recollection of specific injury or trauma. These bruises may take an unusually long time to fade or may appear as clusters of tiny, pinpoint red spots under the skin, known as petechiae. Petechiae are essentially minute hemorrhages caused by capillary bleeding and are particularly concerning because they do not blanch—or turn white—when pressure is applied, unlike a regular rash. Beyond bruising, unexplained nosebleeds, bleeding gums, or excessively heavy menstrual periods in women may also manifest as the first tangible evidence of this underlying clotting deficiency.
These bruises may take an unusually long time to fade or may appear as clusters of tiny, pinpoint red spots under the skin, known as petechiae.
The white blood cells, the body’s primary defense against infection, are also fundamentally compromised by blood cancers, either by being too few in number or by being structurally abnormal and non-functional, as is often the case with leukemia. Consequently, another common early thread in the narrative of blood cancer patients is a pattern of recurrent, persistent, or unusually severe infections. An individual might experience a seemingly endless cycle of colds, sore throats, or respiratory infections that are difficult to treat or take a disproportionately long time to clear. Accompanying this is often an unexplained, low-grade fever that can be intermittent and difficult to pin down. When a fever persists or recurs over days or weeks without a clear source of infection, it may represent a systemic inflammatory response to the proliferation of cancer cells themselves, rather than a mere battle against an external pathogen.
An individual might experience a seemingly endless cycle of colds, sore throats, or respiratory infections that are difficult to treat or take a disproportionately long time to clear.
In the case of lymphomas, which primarily affect the lymphatic system, one of the most classic manifestations is the appearance of painless, persistent swelling of the lymph nodes. Lymph nodes, commonly felt in the neck, armpits (axilla), and groin, are filtering stations for the lymphatic fluid and are often the first place cancerous cells accumulate. While swollen nodes are most often a benign sign of a recent infection, nodes that remain firm and enlarged for several weeks without any concurrent signs of acute illness are a point of serious clinical interest. Particularly worrisome are large, non-tender nodes located in atypical areas, such as above the collarbone (supraclavicular) or in the elbow region. The distinguishing feature here is the lack of tenderness and the duration—benign swelling usually subsides quickly once the infection is cleared, whereas a cancerous node remains a fixture.
Lymph nodes, commonly felt in the neck, armpits (axilla), and groin, are filtering stations for the lymphatic fluid and are often the first place cancerous cells accumulate.
Less frequently discussed, yet highly specific, warning signs include drenching night sweats and unexpected weight loss. Night sweats, particularly those so profuse that they soak through pajamas and bed linens, often occur without an accompanying fever and are recognized as a ‘B symptom,’ a group of systemic indicators common to certain lymphomas. The mechanism is not fully understood, but it is believed to be related to the release of inflammatory chemicals by the cancer cells. Similarly, a noticeable, unexplained loss of body weight—typically defined as more than five to ten percent of total body weight over a six to twelve-month period—without any conscious effort through dieting or increased exercise, may signal that the body is diverting a significant amount of metabolic energy to fuel the rapidly dividing cancer cells, leading to a state of cachexia, or wasting.
Night sweats, particularly those so profuse that they soak through pajamas and bed linens, often occur without an accompanying fever and are recognized as a ‘B symptom.’
Multiple Myeloma, a blood cancer affecting plasma cells in the bone marrow, presents a different set of primary warning signals, often localized initially in the skeletal structure. The accumulation of abnormal plasma cells leads to the destruction and erosion of bone tissue, resulting in persistent and often severe bone pain. This pain is most commonly felt in the back, ribs, or hips, and it frequently intensifies at night or with movement. In more advanced cases, the weakened bones become susceptible to fractures from minimal trauma. The resulting bone destruction can also release excessive calcium into the bloodstream, a condition known as hypercalcemia, which can trigger symptoms like extreme thirst, frequent urination, confusion, and abdominal pain, a complex of symptoms often abbreviated using the acronym CRAB (Calcium elevation, Renal failure, Anemia, Bone lesions).
The accumulation of abnormal plasma cells leads to the destruction and erosion of bone tissue, resulting in persistent and often severe bone pain.
The crucial diagnostic step, which transforms these vague, non-specific complaints into a concrete clinical concern, is the simple yet powerful complete blood count (CBC). When a patient presents with a combination of persistent, unresolving symptoms—fatigue, easy bruising, recurrent fever—the CBC will often reveal aberrations in the number of blood cells: dangerously high or low white blood cell counts, a low hemoglobin level indicative of anemia, and a decreased platelet count. These abnormal cell counts, especially when they are profoundly outside the normal range, provide the first clear, objective evidence that a systemic hematological process is at play, moving the investigation beyond simple primary care diagnoses and necessitating immediate referral to a hematologist for a bone marrow biopsy, which is the definitive diagnostic procedure.
When a patient presents with a combination of persistent, unresolving symptoms—fatigue, easy bruising, recurrent fever—the CBC will often reveal aberrations in the number of blood cells.
It is important to emphasize that none of these symptoms in isolation is pathognomonic—meaning uniquely diagnostic—for blood cancer. The common cold can cause fever and fatigue, minor bumps cause bruises, and anxiety can lead to night sweats. The significant difference, and the signal that warrants further medical investigation, is the persistence of these symptoms and their clustering into a pattern that defies explanation by a more common, self-limiting illness. A cough that lasts three weeks, a bruise that appeared without injury and refuses to fade, or a fatigue that makes it impossible to climb a flight of stairs, particularly when several of these occur together, are the clinical red flags that must not be rationalized away or dismissed as the cost of a busy life.
The significant difference, and the signal that warrants further medical investigation, is the persistence of these symptoms and their clustering into a pattern that defies explanation by a more common, self-limiting illness.
The narrative of early blood cancer signs is one of subtle deviation from baseline health, where minor, seemingly unrelated anomalies accumulate into a chronic, unexplained decline. It demands a partnership between the patient, who must communicate the pattern of their prolonged and non-resolving symptoms, and the physician, who must interpret this clinical narrative not as a series of isolated events but as potential evidence of a fundamental systemic derangement in the body’s blood-forming machinery. Recognizing these initial, often-overlooked signals is the single most effective way to achieve an early diagnosis, which fundamentally alters the therapeutic options and overall prognostic outlook.
Recognizing the subtle, persistent cluster of unusual fatigue, unexplained bruising, and recurrent fevers can be the critical initial step toward diagnosing a hematological malignancy.