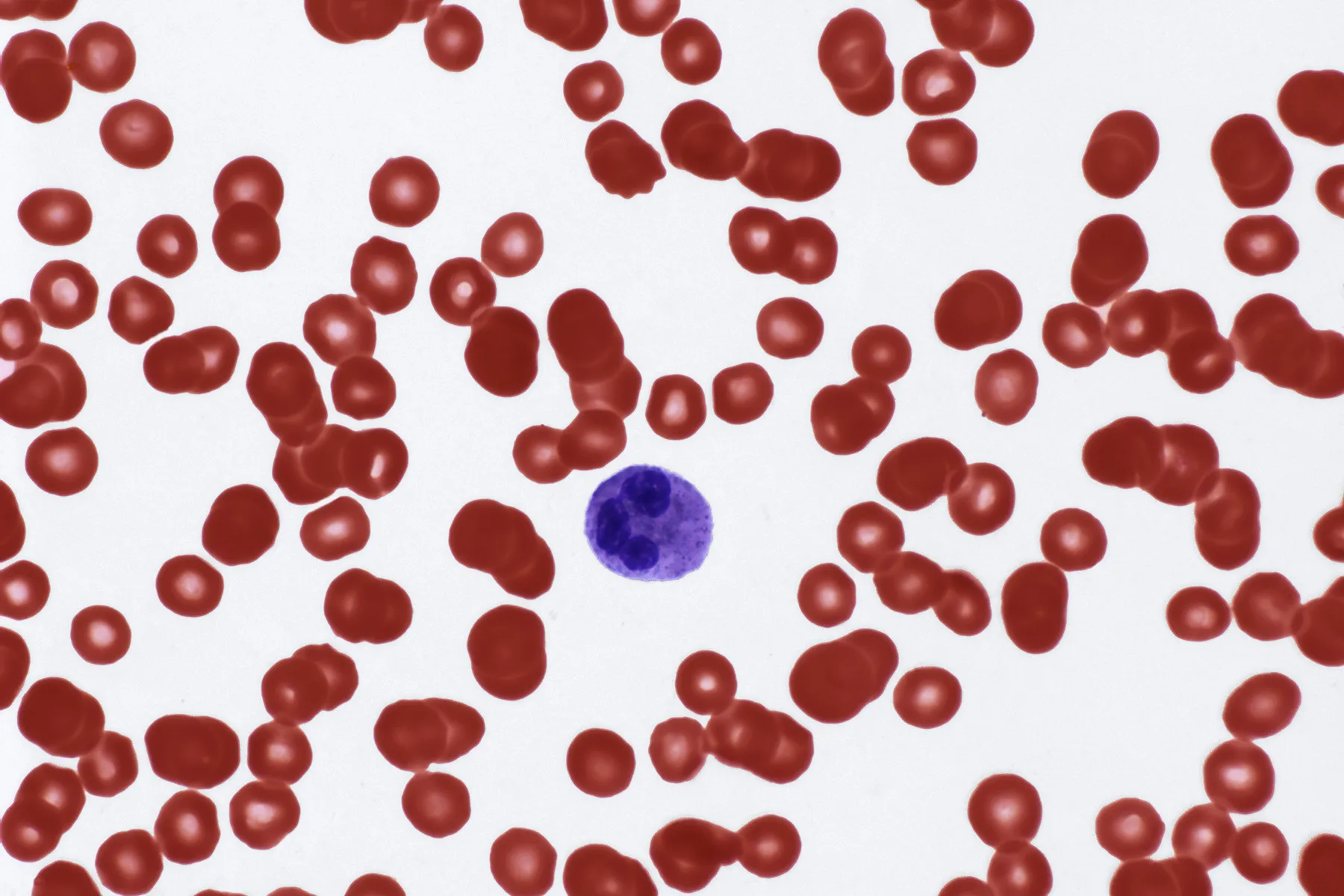
The presence of a diminished white blood cell (WBC) count, medically termed leukopenia, is a significant finding in diagnostic hematology and never an isolated event; it is consistently the outward manifestation of a deeper physiological disturbance. To understand why an individual’s body may be reporting a lower-than-normal concentration of these critical immune cells—primarily neutrophils, lymphocytes, monocytes, eosinophils, and basophils—requires a thorough, investigative approach that spans multiple medical domains. The underlying causes are diverse, ranging from transient infections to profound, systemic diseases that affect the very production factory of blood cells. This complexity in etiology dictates that there is no single answer to the question of what causes a low WBC count, but rather a branching hierarchy of potential explanations rooted in either impaired production, accelerated destruction, or aberrant sequestration of leukocytes.
The underlying causes are diverse, ranging from transient infections to profound, systemic diseases that affect the very production factory of blood cells
The most severe and often concerning causes of leukopenia arise directly from an insult or failure within the bone marrow, the soft, spongy tissue inside bones responsible for all hematopoiesis. This factory of blood cell production is highly susceptible to external damage and internal malignancy. Conditions such as aplastic anemia represent a devastating form of bone marrow failure where the hematopoietic stem cells themselves are destroyed, leading to a simultaneous, dramatic drop in all three blood cell lines: red cells, white cells, and platelets. Furthermore, infiltration of the bone marrow by cancers like leukemia, lymphoma, or metastatic tumors physically displaces the healthy, productive marrow, essentially crowding out the normal process of white blood cell generation, resulting in a persistent leukopenia. This mechanism of diminished production is a primary driver in many of the most serious cases identified.
Furthermore, infiltration of the bone marrow by cancers like leukemia, lymphoma, or metastatic tumors physically displaces the healthy, productive marrow
A less permanent, yet extremely common source of leukopenia lies within the realm of therapeutic interventions, particularly in oncology. Chemotherapy and radiation therapy, designed to eradicate rapidly dividing cancer cells, operate with a lack of specificity that extends their cytotoxic effects to other fast-replicating cells in the body, most notably the myeloid and lymphoid precursor cells in the bone marrow. This intentional suppression, known as myelosuppression, results in a dose-dependent, temporary but often severe drop in white blood cell counts, which typically bottoms out approximately seven to ten days after a treatment cycle. Beyond cancer treatment, a vast number of other pharmacological agents, including certain antipsychotic medications like clozapine, anti-thyroid drugs, specific antibiotics, and immunosuppressants used for transplant and autoimmune disorders, are well-documented to interfere with WBC production or survival, often through unpredictable idiosyncratic reactions. Discontinuation of the offending agent, once identified, often resolves this form of drug-induced leukopenia.
Beyond cancer treatment, a vast number of other pharmacological agents, including certain antipsychotic medications like clozapine, anti-thyroid drugs, specific antibiotics, and immunosuppressants used for transplant and autoimmune disorders, are well-documented to interfere with WBC production or survival
The immune system, in a cruel paradox, can become the agent of its own cellular destruction, leading to a phenomenon called autoimmune neutropenia or leukopenia. In systemic autoimmune diseases like Systemic Lupus Erythematosus (SLE) or Rheumatoid Arthritis (RA), the body mistakenly produces autoantibodies that specifically target and mark the circulating white blood cells for destruction by the spleen or liver. This results in an accelerated destruction or sequestration of the cells faster than the bone marrow can replenish them. The spleen, an organ critically involved in filtering old or damaged blood cells, can become pathologically overactive (hypersplenism) due to underlying liver disease or certain infections, trapping an excessive number of healthy leukocytes and platelets and effectively removing them from circulation, another critical mechanism in the development of low counts.
In systemic autoimmune diseases like Systemic Lupus Erythematosus (SLE) or Rheumatoid Arthritis (RA), the body mistakenly produces autoantibodies that specifically target and mark the circulating white blood cells for destruction
Infectious processes, particularly those of a viral nature, constitute another frequent and often transient cause of a depressed white cell count. Acute viral illnesses, such as influenza, the common cold, or more persistent pathogens like HIV/AIDS and Hepatitis B or C, can temporarily suppress bone marrow activity and alter the distribution of white blood cells within the body’s vascular system, leading to a drop in the measurable count in the peripheral blood. HIV, in particular, selectively attacks and depletes the CD4+ T-lymphocyte subset, leading to a profound and characteristic type of leukopenia (lymphopenia) that cripples the body’s adaptive immune response. Bacterial infections, while typically causing a rise in WBCs (leukocytosis), can in their most overwhelming and severe form—sepsis—cause a paradoxical drop as the demand for neutrophils rapidly outstrips the bone marrow’s supply.
Infectious processes, particularly those of a viral nature, constitute another frequent and often transient cause of a depressed white cell count
Lesser-known but globally significant factors contributing to leukopenia are deficiencies in essential micronutrients, a critical aspect often overlooked outside of comprehensive diagnostic workups. The intricate process of hematopoiesis is metabolically demanding, requiring an adequate supply of various vitamins and minerals to proceed efficiently. Deficiencies in Vitamin B12 and folate, for instance, can lead to megaloblastic changes that impair the final maturation and release of all blood cells, including white cells, from the bone marrow. Similarly, inadequate intake or absorption of trace elements like copper and zinc, which serve as cofactors in numerous enzymatic reactions vital for immune cell function and production, has been scientifically linked to reduced neutrophil counts. Severe malnutrition, regardless of the specific vitamin deficit, can impose a generalized stress on the bone marrow, thus suppressing the overall production of immune cells.
Deficiencies in Vitamin B12 and folate, for instance, can lead to megaloblastic changes that impair the final maturation and release of all blood cells, including white cells
Furthermore, certain rare congenital disorders, passed down genetically, are defined by an intrinsic, often lifelong, failure to produce an adequate number of white blood cells. Kostmann syndrome, for example, is a severe form of congenital neutropenia characterized by a near-complete lack of neutrophils from birth, leaving affected individuals highly vulnerable to life-threatening bacterial infections. These genetic anomalies represent inherent, hard-wired defects in the molecular machinery responsible for the differentiation and maturation of white blood cell precursors, offering a clear-cut case of production failure from the outset of life.
Kostmann syndrome, for example, is a severe form of congenital neutropenia characterized by a near-complete lack of neutrophils from birth
The identification of a low white blood cell count compels a systematic investigation into the patient’s medical history, current medications, exposure history, and lifestyle, as the cause could be an acute, self-limiting viral infection, a side effect of a necessary long-term medication, or the first subtle indication of a serious, developing pathology like a bone marrow malignancy or a previously undiagnosed autoimmune disease. The clinical significance of the finding is determined not just by the degree of the reduction, but more so by the specific type of white cell that is depressed, with neutropenia (low neutrophils) carrying the highest immediate risk for severe bacterial infection. Therefore, understanding the root cause is paramount, as the correct intervention ranges from simple nutritional supplementation to immediate, aggressive treatment of an underlying cancer.
The clinical significance of the finding is determined not just by the degree of the reduction, but more so by the specific type of white cell that is depressed
The complexity of leukopenia’s etiology serves as a powerful reminder of the delicate equilibrium required to maintain a functional immune system. This balance, sustained by the bone marrow’s relentless production line and the body’s regulated disposal and usage of these cells, is susceptible to disruption at almost every point in its cycle. Consequently, a diagnosis of leukopenia is less a definitive end-point and more the crucial start of a detective-like process, with each potential cause—be it a drug, a virus, a nutritional lack, or an autoimmune attack—representing a distinct pathway away from immunological health.